
Medical Microbiology and Infectious Diseases - University of Manitoba
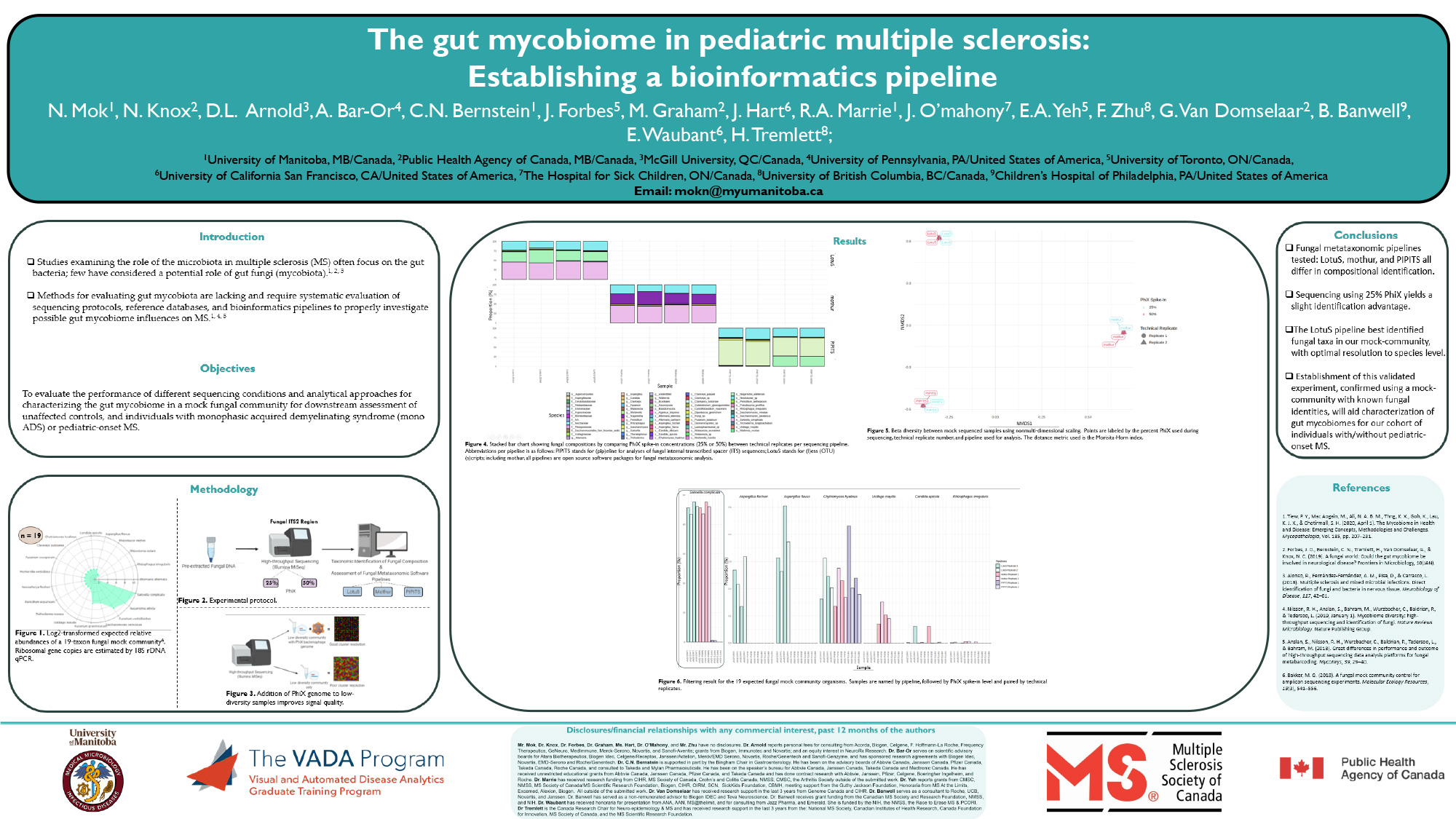
Nelson received his BSc. in 2019, and is currently pursuing his MSc. in Medical Microbiology and Infectious Diseases under the supervision of Dr. Natalie Knox. He will use his knowledge gained from prior work involving bacterial and viral pathogenomics to explore the fungal microbiome in a cohort involving pediatric-onset multiple sclerosis individuals. As a result of the mycobiome being understudied, there is a lack of methodologies, characterization tools, and thorough evaluation of existing protocols; Nelson’s project aims to devise a protocol by evaluating genomic and bioinformatics approaches for examining the gut mycobiota. Further, he will use the established protocol to investigate if an association between the gut mycobiota and multiple sclerosis exists.
Hi Nelson,
Cool work! This is my first time hearing about pediatric onset MS. Do you know if children’s microbiome’s significantly differ from adults? If they differ, is the mock community more similar to the microbiome of adults? If so, how will this affect the ability of the pipeline to identify fungal communities in children?
Hi Sam,
The answer to your question depends on the site of microbiome, as the skin community can differ from the gut or oral communities. In terms of the bacterial gut microbiome, I like to refer to a review by Arrieta et al. (2014), which I read during my undergraduate studies and has stuck with me since. In summary, it depends on the age. At birth, an infants bacterial microbiome differs severely compared to an adult microbiome and this can be due to various factors: delivery method, environment, food, and breast versus formula feeding; however, as an infant ages, their gut community increases in diversity which typically stabilizes at ages 2-3 and carries into adulthood.
Though a direct comparison between a child’s gut microbiome to an adult can give varying results, as this can differ from person to person and use of antibiotics, a general consensus based upon overlapping bacteria suggests a child’s bacterial gut microbiome is less diverse. But if we’re talking about the fungal microbiome, the mycobiome, a paper by Ward et al. (2018) comes to mind. Although this study is very limited in sample size, it looks at the skin, oral, and anal communities. Results indicate that newborns have variable mycobiomes in the first 30 days of life. Also, it does not seem the mycobiome is similar when they compare to their mother’s, but this result is questionable because they compare between two different sites.
At this time, I can’t give you a direct answer if a childs gut mycobiome is similar to an adult because studies about the mycobiome is limited when compared to their baterial counterpart, and this is even more so when studying infants. A contributing factor to a lack of gut fungal microbiome studies is a lack of established analytical protocols, which have been long established for the bacterial microbiome. As such, my study aims to address this problem to further research about the gut mycobiota.
The mock community used in my study does not pertain to the gut mycobiota of adults, it’s more so a mixture of fungi found in the environment to be used as a positive control. This is because mycobiome studies often lack using a proper positive control for validating their results, possibly a contributing factor to why various studies on the same topic differ in results. Also, this mock control serves to determine if popular mycobiome pipelines differ in identification, and helps to further knowledge about fungal metataxanomic tools.